Revolutionizing Pharmacy Benefits by Disrupting the Status Quo and Driving Down Costs, Watch On-Demand
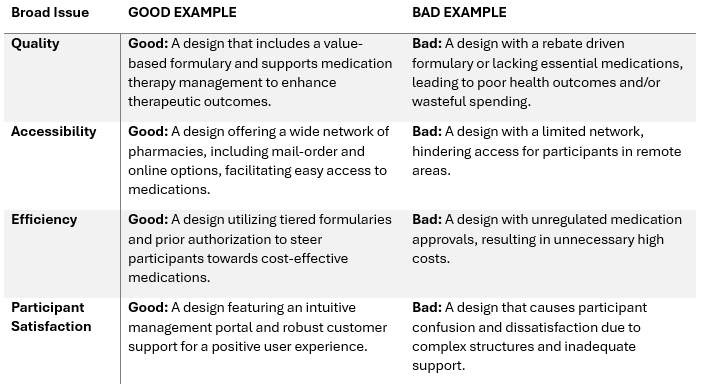
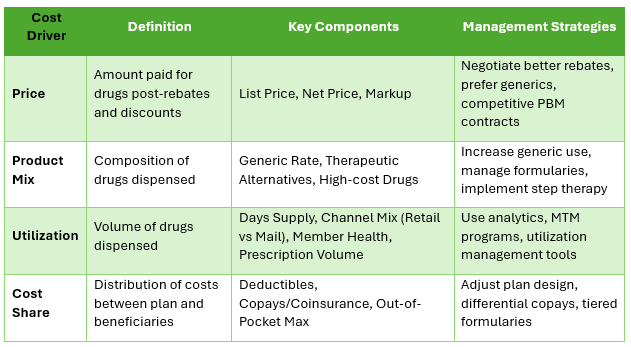
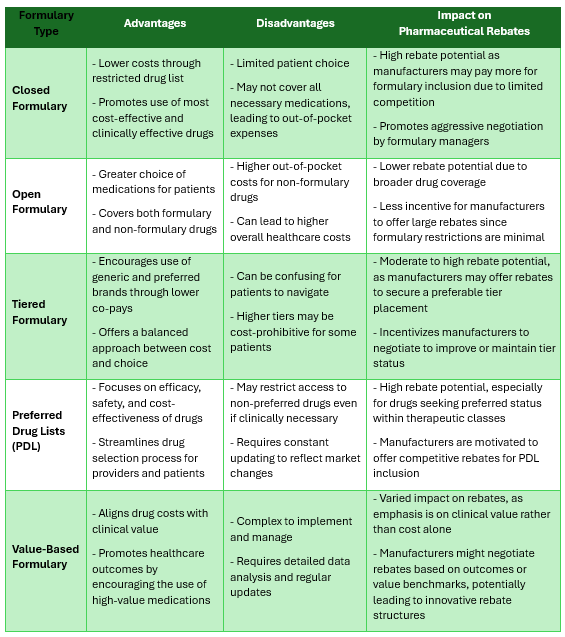
In our webinar, “Revolutionizing Pharmacy Benefits by Disrupting the Status Quo and Driving Down Costs,” we delve into the innovative strategies reshaping the landscape of pharmacy benefits management (PBM). By challenging conventional approaches and implementing cutting-edge solutions, we’re driving down costs while enhancing patient outcomes.
Why You Should Watch:
- Gain Insight: Learn about groundbreaking methodologies transforming pharmacy benefits, equipping you with the knowledge to navigate this evolving industry.
- Cost Reduction Strategies: Discover practical approaches to reducing pharmacy costs without compromising the quality of care, crucial for businesses seeking to optimize their healthcare spending.
- Patient-Centric Solutions: Explore how our innovative techniques prioritize patient well-being, ensuring better health outcomes while containing expenses.
- Industry Disruption: Stay ahead of the curve by understanding the latest disruptions in the PBM sector and how they can benefit your organization.
- Fiduciary Standard of Care: Understand the importance of adopting a fiduciary standard of care in pharmacy benefits management, aligning with best practices and ethical standards.
Who Should Watch:
- Benefits Consultants: Enhance your expertise in PBM to better serve your clients and provide them with actionable strategies to control healthcare costs.
- Human Resources Managers: Gain insights into innovative approaches for managing pharmacy benefits, helping you make informed decisions that benefit your employees and your bottom line.
- Employers: Learn how to optimize your pharmacy benefits program to achieve cost savings while ensuring your employees receive high-quality care.
- Healthcare Professionals: Stay abreast of industry trends and advancements in pharmacy benefits management, enabling you to deliver more effective patient care within your organization.
Watch on-demand as we revolutionize pharmacy benefits together, driving down costs while prioritizing patient well-being. Let’s disrupt the status quo and shape the future of healthcare together!