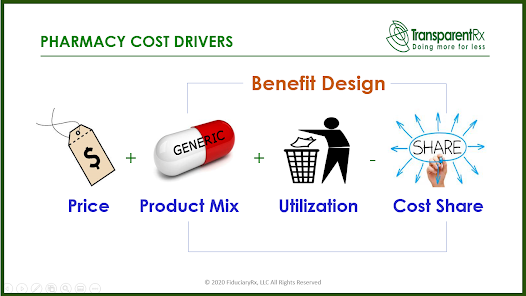
Employer-sponsored plans that prioritize price risk poor clinical outcomes and higher overall costs in their pharmacy programs. Equal focus on all four pharmacy cost drivers will always produce the best results. Price is just one indicator of pharmacy benefits management program success, but it is one that can also hide problems.
On the positive side, lower spend can be the result of better product mix and efficient drug utilization driven by improved formulary management. Here are three myths that have developed in the market and reasons why placing equal emphasis on each of the four pharmacy cost drivers will generate greater value at a lower cost over the long term.
1. Rebates are one of the Top 2 factors in lowering employer-sponsored pharmacy benefit plan costs.” The employer faces a double whammy on rebates: (1) rebates may be kept by the PBM (2) rebates are offered only on expensive drugs. Almost without exception the most heavily advertised and rebated drugs have therapeutic alternatives which cost up to 90% less than the rebated products. An employer may think it need not worry about this structure since it receives 90%+ of the rebates. Are there other fees paid to the PBM by the manufacturer that are relabeled and therefore are no longer considered a “rebate”? Does the employer even have access to the right information to make these decisions?
2. Pass-through and Transparent PBM business models provide similar levels of transparency and price. Non-fiduciary PBM companies have learned how to leverage the purchasing power of the unsophisticated plan sponsor purchaser to their financial advantage. Consequently, pass-through and so called transparent PBM business models don’t let you in on what their management fee amounts to. That is a big big problem. Unlike admin fees, management fees are not easily quantifiable primarily because non-fiduciary PBMs don’t want employer-sponsors to know just how much their fees are contributing to your costs. The full-disclosure and fiduciary-model PBM will disclose to self-insured employers their management fee or the part of negotiated discounts it will keep. The lower this fee the less employers pay plain and simple. A reasonable PBM management fee bends the cost trend whilst delivering similar levels of service and outcomes.
3. Benefit design is less important than pricing guarantees such as AWP discounts and rebates. Never once during hundreds of RFPs has any consultant or broker ever asked us for a signature ready benefit design as part of our response. I’ve not taken a poll so I don’t know the reason. Maybe it is because some believe benefit design doesn’t have a big role in determining cost. If that is the case, nothing could be further from the truth. I would be asking for a benefit design to be submitted as if we were going live with it. In pharmacy cost drivers, price is 1A and benefit design is 1B. Benefit design includes but is not limited to elements such as formulary, network configuration and member cost-sharing arrangements. Aside from copayments and deductibles (cost-sharing) most plan sponsors know little else about their benefit design and have left it up to the PBM to decide. When the PBM is non-fiduciary that could lead to significant overpayments.
There are a lot of bad actors [not just PBMs] in the benefits industry using employers’ bank accounts as their personal ATM. Much can be done by non-fiduciary PBMs to improve the level of transparency provided to purchasers of PBM services. Without a trained-eye reviewing PBM contracts, most companies are at the mercy of PBMs who are essentially given a blank check. I’m not taking purchasers of PBM services off the hook either. Continuous learning is essential to running an efficient and cost-effective pharmacy benefit management program.